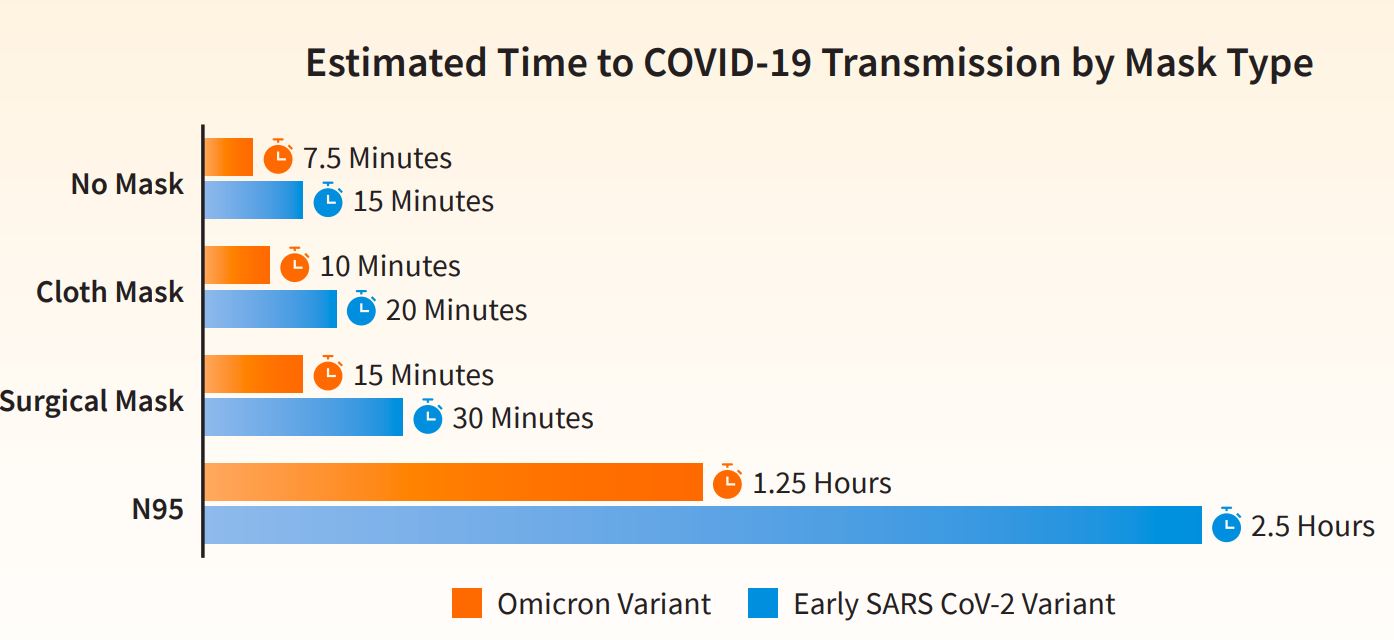
While COVID-19 has waned, it has not yet disappeared. Schools, community leaders, and healthcare providers continue to closely “watch the numbers” to ascertain local infection rates and take actions and precautions accordingly. While they do that, business leaders, especially those in the healthcare industry, continue to watch another indicator—the supply chain and its disruptions.
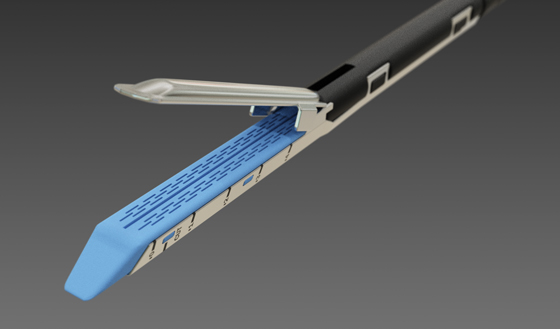
In addition to the pandemic, several other forces have continued to disrupt the supply chain. Recent labor strikes, worker shortages, production slow-downs or stoppages, and war continue to impact the supply chain. To date, the healthcare industry and general public have experienced shortages in personal protective equipment (PPE), baby formula, and now surgical staplers.