All who have cared for our nation’s older adults through the COVID-19 pandemic have given so much; the toll in lives lost, illness, and financial and economic impacts have been great for those we serve, all aspects of the workforce, and provider organizations alike. But the care-critical work is not over.
As the COVID-19 pandemic response and recovery efforts continue worldwide, in our nation, and specifically in the aging services sector it is more important than ever that providers continue efforts to prevent harm to residents, staff, and healthcare partners who care for older adults, and their families and loved ones.
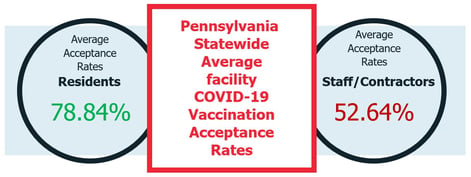
Data from Pennsylvania’s COVID-19 Vaccine Needs Assessment Survey, as shared by the Pennsylvania Department of Health on April 1, 2021, indicates the same trends that other U.S. studies also suggest: a statistically significant lag in COVID-19 vaccination acceptance rates in staff and contractors working in the aging services sector compared to the vaccination acceptance rates of the residents they serve and care for.
“On March 16, 2021 the Acting Secretary of the Pennsylvania Department of Health issued an order requiring skilled nursing facilities to complete the COVID-19 vaccine needs assessment survey.”Vaccine versus Antidote: Not the Same ThingA recent outbreak at a Kentucky nursing home—investigated by the Centers for Disease Control and Prevention (CDC) and described in an April 21, 2021, New York Times article—highlights the risks that unvaccinated staff can bring even to vaccinated residents.
In that outbreak, according to CDC, 26 of the facility's 83 residents and 20 healthcare personnel developed a COVID-19 infection after exposure to an unvaccinated staff member; three of the residents subsequently died. Notably, prior to the outbreak, 90% of the facility's residents had been vaccinated, but only half of its employees had been vaccinated; 22 of the 46 total infections, and one of the three deaths, were in individuals who had been fully vaccinated.
The Times article describes other infections in nursing homes, including a review of 78 Chicago facilities. Emerging fact patterns from these recent outbreak studies indicate the following:
- Even though vaccination rates continue to climb, outbreaks of COVID-19 are still a reality for the aging services sector
- Current vaccines have varying degrees of efficacy against variants of the SARS-CoV-2 virus that causes COVID-19
- Vaccinated persons (residents and staff) may still become infected, but are experiencing less severe illness or may even be asymptomatic
- Vaccinated individuals who become infected can still contribute to a COVID-19 outbreak in aging services facilities
- Those who are not vaccinated and become infected, especially in highly vulnerable groups like older adults, have a greater potential of severe illness, harm, and death
- Lagging COVID-19 vaccination acceptance rates in the aging services workforce can still pose real dangers to residents and others in the workforce
While evidence continues to build regarding the positive effects of vaccination in bringing this pandemic to an end, and of vaccines reducing the effects of COVID-19, it is important not to treat the vaccine as an antidote to becoming infected and ill. Treating vaccination as a sort of force field risks creating a false sense of security and leading to premature loosening of care-critical infection prevention controls. It is only through coupling those infection controls with pandemic response measures like vaccination that preventable harm can be avoided.
Summary
The problems inherent in developing and testing new vaccines for a novel virus and illness, and then executing a nationwide campaign to safely vaccinate the highest number of persons in the shortest amount of time possible, are vastly complex. In addition, the many contributing factors to lagging COVID-19 vaccination acceptance rates in the aging services sector workforce are equally, if not more, complex. Vaccine hesitancy is just one of these factors, but it is a major one that can be addressed by every stakeholder, from healthcare professionals, clinicians, practitioners to public health departments and community leaders from across all of the nation’s federal, state, and community health systems.
During this time it is imperative that we continue to vaccinate the most people possible, which means we must continue to implore all who serve and care for older adults to be vaccinated safely if there are no medically-indicated reasons to decline. This helps all involved meet our obligations as healthcare professionals to do no harm. To accomplish this, we must also acknowledge the realities of vaccination hesitancy by seeking to understand the reasons for declination and continually adapt education, informed consent, and communication programs to help overcome barriers.
In its summary of the Kentucky outbreak, CDC points out the following implication for health practice:
Vaccination of [skilled nursing facility] residents and [healthcare personnel] is essential to reduce the risk for symptomatic COVID-19, as is continued focus on infection prevention and control practices.
CDC's words reflect a tested wisdom, as well as our obligation as healthcare professionals to prevent harm to persons served by not exposing them to infectious disease, not to mention the harm to families and friends that can follow by bringing it home at the end of a shift.
